This topic provides a concise review on anatomy and physiology applied to wound care.
COMMON ANATOMICAL LOCATIONS IN WOUND CARE
Refer to the Quick Reference Tool "Anatomical Locations in Wound Care" below:

Quick Reference Tool: Anatomical Locations in Wound Care (click to enlarge)
ANATOMICAL SYSTEMS
Musculoskeletal System
Muscles
The muscular system is composed of specialized cells called muscle fibers. Their predominant function is contractibility. Muscles, attached to bones or internal organs and blood vessels, are responsible for movement. There are more than 600 muscles in the body, which together account for about 40 percent of a person's weight.[1]
Structure
- Each organ or muscle consists of skeletal muscle tissue, connective tissue, nerve tissue, and blood or vascular tissue. See Figure 1.

Fig. 1. Structure of a skeletal muscle
Bones
Structure
- Consists of cells embedded in an abundant hard intercellular material. The two principal components of this material, collagen and calcium phosphate, distinguish bone from such other hard tissues as chitin, enamel, and shell.[2] Bone tissue makes up the individual bones of the human skeletal system (Figure 2).

Fig. 2. Human skeletal system
CLINICAL APPLICATION
- Pressure Ulcers/Injuries
- PUs/PIs occur over predictable pressure points where bony protuberances are more likely to compress tissues when the patient is in contact with hard surfaces.[3] See Figure 3
- 'Etiology' in "Pressure Ulcer/Injury - Introduction and Assessment"
- 'Pathophysiology' in "Pressure Ulcer/Injury - Introduction and Assessment"
- "Pressure Ulcers/Injuries - Prevention"
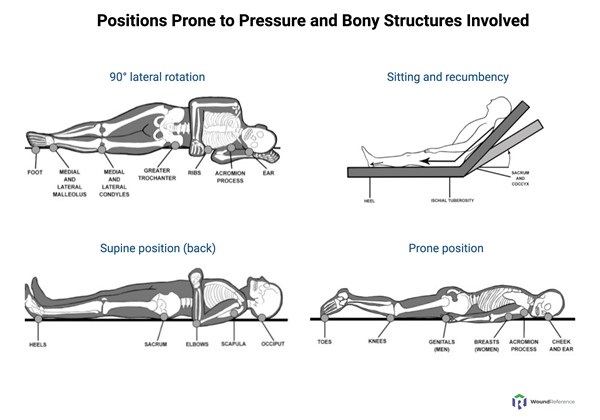
Fig. 3. Positions prone to pressure and bony structures involved
Tendons
structure
- A tendon is composed of dense fibrous connective tissue, composed mostly of water, collagen fibers and glycosaminoglycans (GAGs).[4]
- Primary collagen fibres, which consist of bunches of collagen fibrils, are the basic units of a tendon. Primary fibres are bunched together into primary fibre bundles (subfasicles), groups of which form secondary fibre bundles (fasicles). Multiple secondary fibre bundles form tertiary fibre bundles, groups of which in turn form the tendon unit (Figure 4).
- Endotenon: primary, secondary, and tertiary bundles are surrounded by a sheath of connective tissue (endotenon), which facilitates the gliding of bundles against one another during tendon movement.
- Epitenon: endotenon is contiguous with epitenon, the fine layer of connective tissue that sheaths the tendon unit.
- Paratenon: lying outside the epitenon and contiguous with it is a loose elastic connective tissue layer known as paratenon, which allows the tendon to move against neighbouring tissues. The tendon is attached to the bone by collagenous fibers (Sharpey fibers) that continue into the matrix of the bone.
CLINICAL APPLICATION
- Moisture is important for tendons to remain healthy.
- If properly hydrated and protected, tendons have a glistening white appearance. However, exposed or damaged tendons are prone to infection due to their limited vascular supply, which may also cause tendons to become dry and desiccated (Figure 5).
- Exposed tendons can be identified by moving the joint and watching the tendon glide within its sheath.
- Adequate moisture allows exposed tendons to granulate over and receive collateral capillary support
- For exposed, necrotic tendons, debridement should be conducted by a qualified professional. See topic "How to Perform Conservative Sharp Wound Debridement".

Fig. 4 Tendon anatomy and histology | 
Fig. 5 Venous leg ulcer with exposed tendon |
The Foot
Bones of the foot

Fig.6 Bones of the foot
Compartments of the foot
There are 9 main compartments (controversial) [5][6]
Table 1. Compartments of the Foot
| Compartments | Muscles | Vessels | Nerves |
| Medial | - Abductor hallucis
- Flexor hallucis brevis
|
|
|
| Lateral | - Abductor digiti minimi
- Flexor digiti minimi brevis
|
|
|
| Superficial | Flexor digitorum brevis Lumbricals Flexor digitorum longus tendons |
| |
Interosseous (x4)
| |
|
|
| Adductor | |
|
|
| Calcaneal | | - Posterior tibial artery
- Posterior tibial vein
- Lateral plantar artery
- Lateral plantar vein
| - Posterior tibial nerve
- Lateral plantar nerve
- Medial plantar nerve (?)
|
Vascular System
Figure 7 illustrates the arterial and venous systems.

Fig.7. Arterial and venous systems
Upper extremity
Arterial anatomy
The main upper extremity arteries are [7]:
- Subclavian artery: vascularizes the arm. It is a branch of the aorta on the left side, while on the right, it is one of the terminal branches where the brachiocephalic trunk bifurcates.
- Axillary artery: it is the continuation of the subclavian artery, from the first rib’s lateral edge to the pectoralis major muscle’s inferior border. As the subclavian artery, it is a short artery.
- Brachial artery: greater in length, it continues to the axillary artery and paves a route along the whole arm’s inner face. It bifurcates in the antecubital fossa, giving two terminal branches: radial and ulnar artery. In up to 15% of cases, it can present an anomaly consisting of a proximal bifurcation, which will cause the existence of a double artery in the arm.
- Radial artery: it is the brachial artery’s terminal branch, which presents a relatively deep first segment, is placed in a more superficial position. It approaches the hand and follows the radial edge of the forearm (pulse channel). The radial artery can be identified from its origin because it is the most superficial artery after the brachial artery’s bifurcation.
- Ulnar artery: it is the other terminal branch of the brachial artery, which, like the radial, follows a relatively deep path at the beginning but is located superficially in the wrist. Typically, it branches into a collateral at a short distance from its origin, the interosseous artery.
- Palmar arch: it represents the terminal anastomoses between the radial and ulnar arteries. The palmar arch shows great variability. Usually, it consists of two arches: the deep palmar arch, mainly dependent on the radial artery, which anastomoses with the ulnar artery; and the superficial palmar arch, tributary to the ulnar, which anastomoses with the radial artery.
Venous anatomy
In upper limbs, venous drainage occurs in two main systems: superficial and deep venous systems [7] :
Deep venous system [7]:
- Veins of the deep venous systems are located alongside the main trunk arteries and have the same corresponding names (radial, ulnar, brachial, axillary and subclavian veins)
- They are usually in even numbers, so that two veins accompany each artery.
Superficial venous system [7]:
- Consists of two drainage systems: the cephalic vein and the basilic vein, and collects the venous drainage from superficial tissues and drains into the deep venous system.
- Cephalic vein: responsible for superficial venous drainage and follows a path along the forearm’s radial edge, external arm face and deltopectoral groove. It is the longest vein in the upper limb. Its trajectory follows the most superficial path of all the trunk veins, so it is the first-choice vein to try to create vascular access.
- Basilic vein: follows a trajectory in the ulnar portion in the forearm. While in the arm, it is located in the inner face, close to the brachial vascular sheath package. Although its deeper location often preserves it from injuries due to iatrogenic puncture, it is the second-choice vein for vascular access after the cephalic vein.
Lower extremity
ARTERIAL ANATOMY
The main lower extremity arteries are [8]:
- Common Femoral Artery (CFA): continuation of the external iliac artery. The CFA courses anterior to the femoral head and divides into the deep femoral artery (profunda femoris) and superficial femoral artery (SFA).
- The SFA continues distally through the adductor canal and becomes the popliteal artery at the adductor hiatus. The SFA supplies blood to the lower leg while the deep femoral artery supplies blood to the hip and thigh.
- The deep femoral artery branches into medial femoral circumflex, lateral femoral circumflex, and terminal perforating vessels.
- Popliteal Artery: travels within the popliteal fossa and bifurcates into the anterior tibial artery and tibioperoneal trunk. The tibioperoneal trunk then divides into the posterior tibial artery and peroneal (fibular) artery.
- Anterior Tibial Artery: the anterior tibial artery supplies the anterior compartment of the lower limb. At the anterior ankle, it becomes the dorsalis pedis artery. It subsequently branches into the medial malleolar, lateral malleolar, medial tarsal, lateral tarsal, and arcuate arteries.
- Posterior Tibial Artery: the posterior tibial artery travels within the deep posterior compartment of the leg along the border with the superficial compartment. At the level of the ankle, it travels posterior to the medial malleolus and into the tarsal tunnel. It gives off the medial plantar, lateral plantar, and medial calcaneal arteries.
- Peroneal Artery: the peroneal artery arises from the tibioperoneal trunk and supplies the muscles of the lateral compartment of the lower leg (peroneus brevis, and peroneus longus).
Venous Anatomy
The lower extremity venous system is traditionally divided into the superficial and deep systems, according to the relationship to the muscular fascia (Figure 8). [9]
- Superficial veins lie above the muscular fascia and drain the cutaneous microcirculation.
- Deep veins lie beneath the muscular fascia and drain the lower extremity muscles.

Fig. 8. Schematic illustrating a cross sectional view of the lower extremity venous system (superficial and deep compartments)
Superficial venous system
The two major superficial veins of the lower extremities are the great saphenous vein (GSV) and small saphenous vein (SSV).[10] (Figure 9)
- Great saphenous vein (GSV): arises from the medial aspect of the dorsal pedal venous arch, ascends anteriorly to the medial malleolus, passes posteromedially to the knee, and ascends medially in the thigh to join the common femoral vein through the saphenofemoral junction. Throughout its path, the GSV receives several tributaries (e.g. the posterior accessory saphenous vein).
- Small saphenous vein (SSV): arises from the dorsal pedal arch and ascends along the middle of the calf and ends in the popliteal vein through the saphenopopliteal junction (SPJ).
- Before it penetrates the muscular fascia, the SSV may branch out a cranial extension, known as the vein of Giacomini, which goes upward to join the GSV. This vein has been found by duplex examination in 70% of limbs with chronic venous insufficiency.[11]
- Gross incompetence of the SSV typically only arises in regions where the SSV and its contributing veins lie above the deep fascia, that is, on the lateral calf and lower third of the leg behind the lateral malleolus.[11]
Duplex ultrasound (DUS) imaging made it easier to visualize anatomical details first described in the early nineteenth century by French anatomists Cruveilhier and Bayle [11][12][13]:
- The subcutaneous space containing all superficial veins is divided by the superficial (membranous) fascia into two layers (Figure 8):
- Superficial layer: loculated fatty subcutaneous tissue (an extension of Camper fascia found in the abdomen).
- Deep layer: collagen and elastic tissue providing strong support (an extension of Scarpa fascia found in the abdomen).
- The superficial fascia serves as a marker to distinguish between the two levels of superficial veins:
- Both saphenous veins (GSV and SSV) are located in the deeper compartment of the subcutaneous space, and are covered for their entire length by the superficial fascia. Other veins in the same intrafascial compartment include:
- Proximal part of the Anterior Accessory Saphenous Vein (AASV)
- Medial and lateral marginal veins of the foot.
- Dorsal foot arch.
- Other superficial veins, including tributaries or collaterals of the saphenous, are situated in the superficial compartment, between the superficial fascia and skin.
Deep venous system
The major deep veins of the lower extremities follow the course of the corresponding arteries (Figure 9).[10] Each of the three arteries in the leg - the anterior and posterior tibial arteries and the peroneal artery - is accompanied by at least two deep veins. These veins are interconnected through transverse links, forming a structure similar to a ladder.[11]
- Foot:
- Dorsal venous arch: mostly drains into the superficial veins
- Medial and lateral plantar: combine to form the posterior tibial and peroneal veins
- Calf: the deep venous system of the calf includes the following deep veins, which present as pairs on both sides of the artery:
- Anterior tibial
- Posterior tibial
- Peroneal veins
- Knee:
- Popliteal vein: formed by the junction of the anterior and posterior tibial veins at the lower aspect of the posterior knee
- Thigh:
- Femoral vein: after the popliteal vein goes into the adductor hiatus, it is referred to as the femoral vein (the term superficial femoral vein is no longer recommended, because this vein is not a superficial vein, but rather a deep vein)
- Deep femoral vein: runs along the deep femoral artery,
- Common femoral artery: results from the junction of the femoral vein and the deep femoral vein, and it is located medial to the common femoral artery.
- Groin: the inguinal ligament is the landmark that divides the common femoral vein from the external iliac vein
Other types of veins of the lower extremity include:
- Perforating veins: perforating veins penetrate the muscular fascia and connect the superficial and deep veins.
- Communicating veins: are veins that connect veins within the same system (i.e., deep to deep, superficial to superficial).

Fig. 9. Veins of the lower extremity
CLINICAL APPLICATION
- Venous leg ulcers:
- See sections 'Etiology and Pathophysiology' in topic "Venous ulcers - Introduction and Assessment"
- Muscle pump: In comparison with arteries, veins have a weaker muscular layer and less elastic tissue. The high capacitance of the venous system is critical to the function of the calf “muscle pump”. See how the muscle pump works in topic "Compression Therapy".
- Valves and venous return:
- The superficial, deep, and most perforating veins contain bicuspid valves formed from folds of endothelium supported by a thin layer of connective tissue. In the lower extremities, the valves function to ensure flow from superficial to deep and from caudal to cephalad directions. The lower extremity valve cusps remain open during rest in the supine position. Valve closure is a passive event initiated by reversal of the resting antegrade transvalvular pressure gradient. As the pressure gradient is reversed, there is a short period of retrograde flow, or reflux, until the gradient becomes sufficient to cause valve closure.
- In venous disease, valves often become incompetent leading to venous reflux and hypertension. See topic "Compression Therapy".
- CEAP: Clinical guidelines recommend documenting the level of venous insufficiency with a standardized score such as the CEAP (Clinical-Etiology-Anatomy-Pathophysiology) classification system. See section 'CEAP Classification System' in topic "Venous ulcers - Introduction and Assessment"
- Vascular Surgical Interventions: see topic "Venous Ulcers - Treatment and Prevention"
- Arterial ulcers:
- See sections 'Etiology' and 'Pathophysiology' in topic "Arterial Ulcers - Introduction and Assessment"
- Angiosomes: according to this concept, the location of an ulcer may offer a hint on which arteries are affected by stenosis or occlusion, in light of the corresponding angiosome. See 'Angiosome Mapping' in topic "Arterial Ulcer - Introduction and Assessment".
- "Arterial Ulcer - Surgical Treatment"
Lymphatic System
Structure
- The lymphatic system consists of lymphoid organs (spleen, thymus, tonsils, Peyer's patches, bone marrow), lymph nodes, MALT (Mucosal Associated Lymphoid Tissue), and lymphatic vessels.[14] See Figure 10.
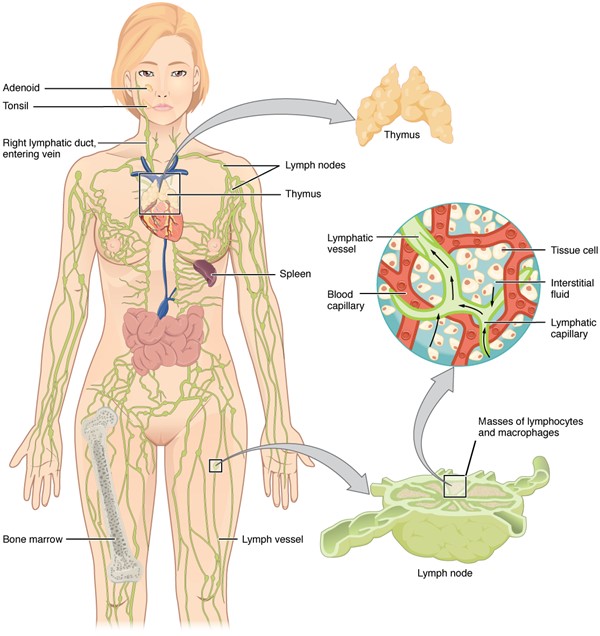
Fig. 10. Anatomy of the lymphatic system, composed of lymph nodes, lymphatic collecting vessels and associated lymphoid organs
Function
- Roles of the lymphatic system: vary from maintenance of tissue fluid homeostasis by clearing interstitial fluid of water, lipids (long fat-chain fats), and plasma proteins, to immune cell and antigen transport between the periphery and central lymphoid tissues.[15] See short video on lymphatic system in topic "Lymphedema - Introduction to the Lymphatic System"
- Differences compared to the cardiovascular system: Unlike true circulatory systems, the lymphatic system is an open-loop low-pressure circuit with no central pump. The lymphatic system is composed of multiple structures (Figure 11) [14][16]:
- Lymph nodes (Figure 11): contain lymphocytes and leukocytes that provide immune function and filter lymphatic fluid.
- Lymphatic vessels (Figure 11): vessels with valves that provide unidirectional lymph fluid flow throughout lymphangions (i.e, segments between valves, which comprise a lymphatic vessel, the "lymph micro heart"), conducting lymph to the venous system. Lymph flow is facilitated by neighboring muscle contraction and arterial pulsations. Lymphatic vessels also participate in the formation of lymph.
- Lymph trunks are valvular conducting vessels that return lymph to the venous system's thoracic duct.[16]
- Lymph collectors transport lymph fluid to the lymph nodes and the lymphatic trunks. They are valvular and function as drains. Collectors are divided into valve segments (lymphangions). They are surrounded by a layer of smooth muscle that is autonomically innervated.[16]
- Lymphangions are the lymph micro hearts. Their ability to contract (known as lymphangiomotoricity) is affected by intrinsic and extrinsic factors.
- Intrinsic factors: autonomic. Spontaneous rhythmic contractions at a rate of 6-12 per minute at rest.
- Extrinsic factors:
- Contraction of muscle/ exercise
- Arterial pulsation
- Respiration
- Compression (bandage/garment)
- Manual lymph drainage (MLD). See topic "Lymphedema - Treatment and Emerging Strategies for Prevention".
- Lymphatic capillaries (Figure 11): made up of lymphatic endothelial cells separated by gaps, allowing the passage of larger molecules that would not enter blood capillaries. Lymphatic capillaries originate in interstitial connective tissue and are avalvular. Anchoring ligaments attached to a single endothelium layer open overlapping flaps which allows fluid to move from the interstitial space into the lymphatic capillary, where it becomes lymph.[16] The lymphatics, not the venules, are predominantly responsible for maintaining tissue fluid balance by absorbing interstitial fluid and ultimately returning it into the circulation.[17]
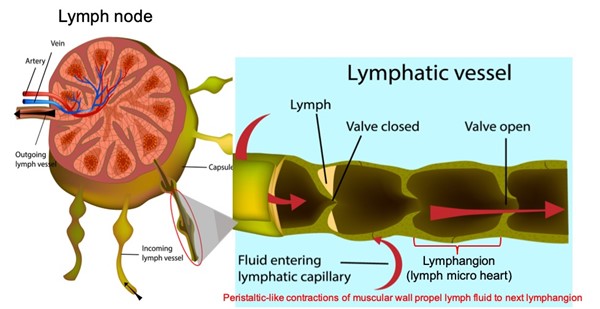
Fig. 11. Lymph node and incoming lymph vessel, demonstrating how a lymphangion directs lymphatic flow
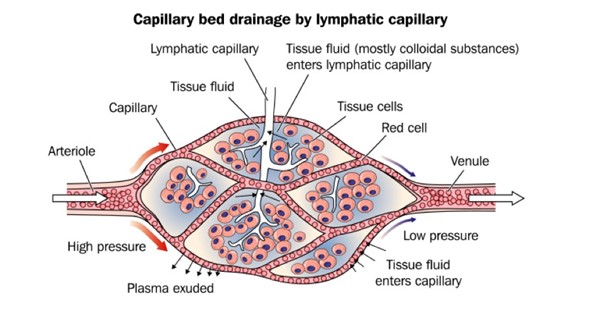
Fig. 11. Lymphatic capillary (white capillary in the center) collects larger molecules that would not enter blood capillaries (red)
Clinical Application
- Lymphedema
- See 'Etiology' and 'Pathophysiology' in topic "Lymphedema - Introduction and Assessment".
- Phlebolymphedema: is a swelling of mixed etiology that occurs as a result of the lymphatic system's inability to adequately drain interstitial fluid associated with chronic venous hypertension. See 'Etiology' in topic "Lymphedema - Introduction and Assessment".
- See topic "Lymphedema - Surgical Management".
Neurological System
Upper Extremity
The major nerves of the upper extremity are [18]:
- Brachial plexus: the brachial plexus is a group of nerves that control the muscles of the shoulder, arm, forearm, and hand. These same nerves also provide sensations of the whole upper limb. There are five components of the brachial plexus: roots, trunks, divisions, cords, and branches.[18]
- Peripheral nerves (see Table 2)
Table 2. Major peripheral nerves of the upper extremity
| Nerve | Motor function | Sensation |
Axillary | - Teres minor and deltoid muscles
| |
Musculocutaneous
| - Brachialis, biceps and coracobrachialis muscles
| - Lateral half of forearm and lateral portion of posterior forearm
|
Medial
| - Forearm flexors, thenar muscles and lateral two lumbricals
| - Lateral part of palm and lateral 3 and a half fingers
|
| Radial | - Triceps and extensor muscles of posterior compartment
| - Posterior arm and forearm and posterior lateral aspect of hand
|
Ulnar
| - Forearm muscles that bend the tips of the small and ring fingers (the flexor digitorum profundus) and also one of the muscles that bends the wrist (the flexor carpi ulnaris).
- Almost all of the small muscles in the hand (including the hypothenar muscles, the lumbricals to the ring and small finger, the palmar and dorsal interossei muscles, the adductor pollicus, and the deep head of the flexor pollicus brevis), except thenar and lateral two lumbricals.
| - Small finger side of the palm, the small finger, and the side of the ring finger next to the small finger. It also provides sensation to the back of the small finger side of the hand.
|
Lower Extremity
The major nerves of the lower extremity are [19]:
- Lumbar plexus: the lumbar plexus supplies innervation to the femoral (L2 through L4), lateral femoral cutaneous (L2, L3), obturator (L2 through L4), and saphenous nerves (L2 through L4)
- Sacral plexus: the sacral plexus gives rise to the sciatic nerve (L4 through S3), posterior femoral nerve (S1 through S3), superior gluteal nerve (L4 through S2), and inferior gluteal nerve.
- Peripheral nerves (See Table 3)
Table 3. Peripheral nerves of the lower extremity [19]
| Nerve | Motor function | Sensation |
Femoral (derived from L2-L4) | - Pectineus, iliacus, sartorius, quadriceps femoris
| - Anteromedial aspect of thigh and medial thigh and leg
|
Obturator | - Medial adductor compartment of thigh
| |
Sciatic | - Posterior thigh and hamstring portion of adductor magnus
| |
Tibial | - Posterior compartment of leg
| - Posterolateral side of leg, lateral foot and sole
|
Common peroneal | - Short head of biceps femoris
| - Upper lateral and lower posterolateral leg
|
Superficial peroneal | - Lateral compartment of the leg
| - Dorsum of foot and anterior and lateral portion of inferior third of leg
|
Deep peroneal | - Anterior compartment of the leg and some foot intrinsics
| - Triangular region of skin between first and second toes
|
CLINICAL APPLICATION
- Diabetic Foot Ulcers
- See 'Etiology' and 'Pathophysiology' in topic "Diabetic Foot Ulcers - Introduction and Assessment".